Data table
View data tableNote
Includes suicide (attempted) and purposedly self-inflicted poisoning or injury. Hospital separations were classified using ICD-9-CM up to 1997-98 and ICD-10-AM from 1998-99 onwards. Rates were age-adjusted using the Australian population as at 30 June 2001. Numbers for 2006-07 include an estimate of the small number of interstate hospitalisations, data for which were unavailable at the time of production.
Source
NSW Admitted Patient Data Collection and ABS population estimates (HOIST). Centre for Epidemiology and Research, NSW Department of Health.
Commentary
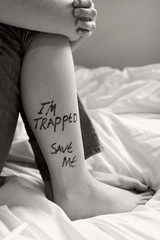
Completed suicide is only one outcome of intentionally self-harming behaviours.
One other outcome of these behaviours is hospitalisation. It is not accurate to regard hospitalised self-harm as equivalent to 'attempted suicide' for comparison with 'completed suicide'. There is some overlap between hospitalised self-harm and suicide, as some suicide deaths occur after admission to a hospital, however, hospitalised self-harm is more frequent than completed suicide. (Steenkamp et al, 2000).
Most people who contact health services after an episode of intentional self harm are seen by emergency departments. They may or may not be admitted as hospital inpatients, and the injury may or may not be recorded as intentional. In recent years, there have been more than 10,000 hospital separations per year following an episode of intentional self harm.
Hospitalisation rates for intentional self-harm are consistently higher in females than in males, while the death rates from suicide are about 3 - 4 times greater in males than in females. This is thought to be mostly due to males using more lethal methods than females. The numbers of young females aged 15-24 hospitalised for self harm has begun to decrease after a peak in 2004-05 (483.0 per 100,000 in 2004-05), however the numbers remain significantly higher than among any other age group (435.6 per 100,000 population compared to 185.3 per 100,000 for females of all ages in 2006-07).
For more information
NSW Department of Health. Suicide prevention in NSW. Sydney: NSW Department of Health, 2003. Available at www.health.nsw.gov.au/pubs/s/pdf/well_suicide.pdf.
NSW Government New South Wales Interagency Action Plan for Better Mental Health Sydney: Available at http://www.dpc.nsw.gov.au/__data/assets/pdf_file/0015/11490/interagency.pdf
NSW Department of Health. Policy guidelines for the management of patients with possible suicidal behaviour for NSW Health staff and staff in private health facilities. Sydney: NSW Department of Health Circular 92/31, 1998.
Pirkis J, Burgess P, Dunt D. Suicidal ideation and suicide attempts among Australian adults. Crisis 2000; 21: 16-25.
Steenkamp M, Harrison J. Suicide and hospitalised self-harm in Australia. Injury Research and Statistics Series. AIHW Catalogue no. INJCAT 30. Adelaide: Australian Institute of Health and Welfare, 2000.
Steenkamp M, Harrison J. Suicide and hospitalised self-harm in Australia. Injury Research and Statistics Series. AIHW Catalogue no. INJCAT 30. Adelaide: Australian Institute of Health and Welfare, 2000.
Australian Government of Health and Aged Care's suicide prevention information available at Suicide prevention, national suicide prevention strategy www.health.gov.au/internet/wcms/publishing.nsf/Content/mental-suicide and at Healthinsite www.healthinsite.gov.au/topics/Suicide_Prevention.
Print version with data
Although this page can be printed directly from your Web browser, a higher quality version of this entire page (graph, table and text) is available as an Acrobat PDF file which can be printed or viewed on screen using free software.
Downloadable files
The data contained in the table on this page are available for download as a CSV file which can be imported into many software packages. The graph is available for download as an EPS (Encapsulated PostScript) file and as an EMF (Enhanced Metafile Format) file. Files in these formats can be imported into most word processing, presentation and graphics software packages.
Copyright notice
This work is copyright NSW Department of Health, 2006. It may be reproduced in whole or in part, subject to the inclusion of an acknowledgement of the source. Commercial usage or sale is prohibited.
Suggested citation
Population Health Division. The health of the people of New South Wales - Report of the Chief Health Officer. Sydney: NSW Department of Health. Available at: www.health.nsw.gov.au/publichealth/chorep/. Accessed (insert date of access).
Produced by
Centre for Epidemiology and Research, Population Health Division, NSW Department of Health.
Last updated on 15 December 2008